The shoulder joint is one of the most mobile joints in the human body. This wide range of motion can, over time, cause the joint surfaces to wear down and the cartilage (the smooth tissue covering bone-ends) to deteriorate. This condition is called shoulder osteoarthritis, also known as “wear-and-tear” arthritis. As the osteoarthritis progresses, it results in shoulder pain, limited range of motion (stiffness), and difficulty performing daily activities.
Shoulder osteoarthritis is most commonly seen in individuals over the age of 50. The most frequent cause is age-related cartilage degeneration (the breakdown of joint-cushioning tissue). In addition, previous traumas (injuries), shoulder dislocations, rheumatic diseases (like rheumatoid arthritis), and rotator cuff tears can also lead to osteoarthritis in the shoulder joint. Over time, patients may find it difficult to perform simple actions such as putting on a shirt, combing their hair, or making overhead movements.
Conservative methods (non-surgical treatments) such as medication, physical therapy, and intra-articular injections (shots directly into the joint) may provide initial relief. However, in advanced-stage shoulder osteoarthritis, these methods become inadequate. When pain and limited motion become severe, total shoulder replacement surgery (also called total shoulder arthroplasty) is recommended.
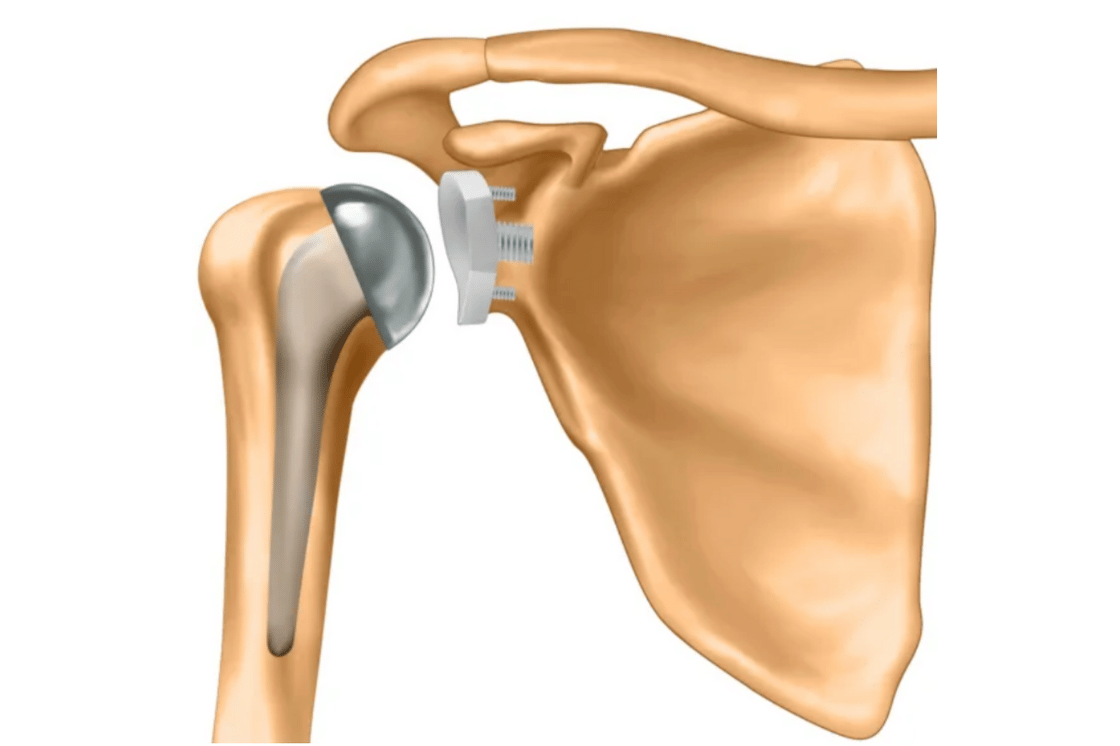
A total anatomical shoulder replacement involves replacing the damaged joint surfaces with an artificial joint (a prosthesis) made of metal and polyethylene (a medical-grade plastic) components. This prosthesis is designed to mimic the shoulder’s natural anatomy, which helps to reduce the patient’s pain and restore the shoulder’s range of motion. An anatomical prosthesis is the preferred option, especially for patients who have intact rotator cuff muscles.
Patients experience relief and a painless shoulder shortly after surgery. With a recovery process supported by physical therapy, the shoulder’s functions are largely restored. The success rate is significantly high with appropriate patient selection and the correct surgical technique.

Surgery Duration: Approximately 90–120 minutes
Type of Anesthesia: A combination of general anesthesia and a nerve block (an injection to numb the shoulder area)
Surgical Method: Open surgery (with an incision, or cut, on the front of the shoulder)
First day: 4–6 (or 2–3 if a nerve block is used)
First week: 3–4
After the 2nd week: 1–2
A hospital stay of 2 nights is generally recommended
First 4 weeks: The shoulder is protected with an arm sling
Starting from the 2nd week: Passive movements (where a therapist gently moves your arm) begin
Weeks 4–6: Active movements (moving your own arm) and strengthening exercises
3rd month: Return to daily life and functional activities 6th month: Clearance for sports and heavy loading
First dressing change: 2nd day
Wound check: 1st week Stitches (sutures) are removed on the 10th day, if necessary
Modern prostheses generally last for 15–20 years or longer. With proper use and follow-up, they can remain functional for a lifetime.
For the vast majority of patients, pain is significantly reduced or disappears completely. Range of motion is also substantially regained.
The arm is protected with a sling for the first 4 weeks. After the 2nd week, controlled exercises are started to restore range of motion. Functional use is typically achieved within 6–12 weeks.
The surgical incision (cut) is made on the front of the shoulder and is carefully closed for aesthetic reasons. The scar will fade over time.
The risk of loosening is low for prostheses placed with the proper surgical technique. However, it is recommended to avoid heavy loading and trauma (impact or injury) to the shoulder.