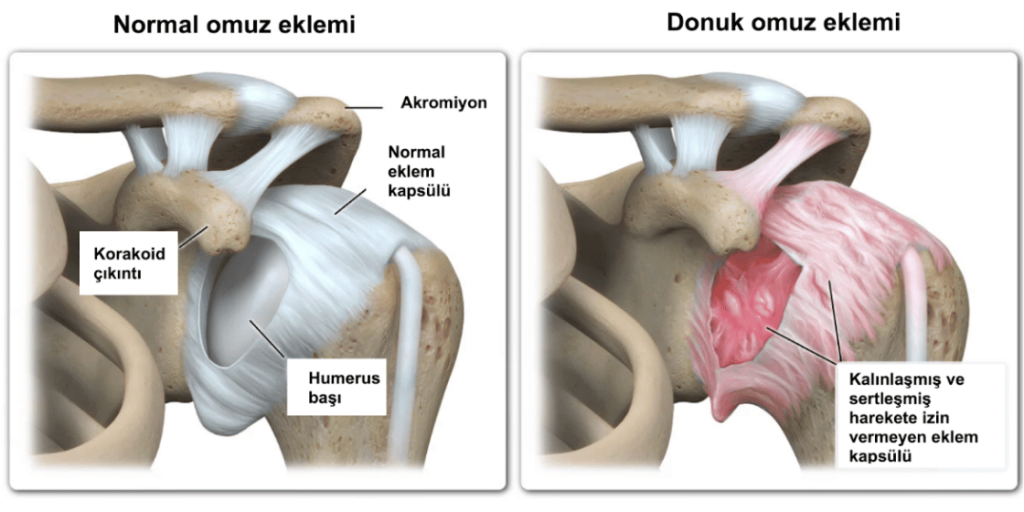
Frozen shoulder, medically known as adhesive capsulitis, is a condition caused by the thickening and tightening of the capsule tissue surrounding the shoulder joint, which severely restricts shoulder movement. This condition typically develops slowly and can progress to a state of almost complete immobility of the shoulder, accompanied by increasing pain over time.
While the exact cause of frozen shoulder is not always clear, it is more commonly seen in patients with diabetes, thyroid disorders, individuals who have been unable to use their shoulder for a long period, or following previous trauma or surgery. The condition generally appears in individuals between the ages of 40 and 60 and is slightly more common in women.
The disease process usually progresses in 3 stages:
In most cases of frozen shoulder, recovery can be achieved over time with physical therapy and pain management. However, in some patients, the restriction of movement becomes permanent or can last for years. In such situations, surgical treatment becomes an option.
Arthroscopic capsular release (minimally invasive or ‘keyhole’ surgery) is one of the most effective surgical treatments for frozen shoulder. In this technique, small incisions are used to access the shoulder joint, and the thickened, scarred capsule tissue that has formed adhesions (stiff bands of tissue) is carefully cut. This procedure frees the joint, allowing the shoulder to begin moving again.
Thanks to this minimally invasive method, the recovery process is more comfortable and faster. Physical therapy begins immediately after surgery to maintain and enhance the range of motion and build strength. When performed at the right time and on the right patient, the surgery yields highly successful results.
Surgery Duration: Approximately 45–60 minutes
Type of Anesthesia: A combination of general anesthesia and a nerve block (an injection to numb the area)
Surgical Method: Minimally invasive (arthroscopic), performed through small incisions of 3–4 mm
First day: 4–5 (or 1–2 with the nerve block)
First week: 3–4
After 2 weeks: 1–2
A hospital stay of 2 nights may be required to allow for physical therapy to be administered during the admission.
First day after surgery: Physical therapy begins
First 3 weeks: Exercises to maintain range of motion
3–6 weeks: Active movement and strengthening exercises
2nd–3rd month: Full return to daily activities
3rd–6th month: Return to sports and high-effort activities
First dressing change: On the 2nd day
Wound check: In the 1st week
Stitches: Stitches, if any, are removed on the 10th day
Yes, some cases do resolve on their own over time. However, this process can take 1–2 years, and the loss of movement may become permanent. Therefore, surgery is recommended if the recovery process is prolonged.
The surgery releases the adhesions (stiff tissues), but achieving full range of motion requires the help of physical therapy. A significant gain in movement becomes noticeable within a few weeks.
Regular physical therapy is generally required for 1-2 months. This duration can vary depending on the patient's age, the severity of the shoulder stiffness, and their muscle structure.
For the vast majority of patients, the pain decreases significantly. Night pain improves rapidly, but complete relief may take a few weeks.
Recurrence is rare. However, if the patient does not adhere to the physical therapy program, some of the movement restriction can partially return.